The Benefits of Telemedicine
Workers’ Comp Via Remote Access
Nevada is considering implementing rules pertaining to the use of telemedicine in the state’s workers’ comp system. It is among just a few states to do so.
Advocates say telemedicine could address several challenges in the workers’ comp system, especially cost and access to care. With the potential shortage of physicians to care for injured workers stemming from the implementation of the Affordable Care Act, some say the time is ripe for the system to embrace the opportunities telemedicine creates.
The Scope of Telemedicine
“Broadly defined, telemedicine is basically the delivery of health care using telecommunications technology,” explained Jonathan Linkous, the CEO of the American Telemedicine Association. “The key is the delivery of health care. It’s not an administered internal system in a hospital; it is not an X-ray machine or an electronic health record. It is actually providing services to a real person at a distance.”
Telemedicine can include a variety of services. The ATA identifies the following examples of delivery systems that can be used:
- Networked programs that link tertiary care hospitals and clinics with outlying clinics and community health centers in rural or suburban areas, using dedicated high-speed lines or the Internet for telecommunication links between sites. The ATA estimates there are approximately 200 such networks in the U.S. providing connectivity to over 3,000 sites.
- Point-to-point connections using private, high-speed networks that are used by hospitals and clinics that deliver services directly or outsource specialty services to independent medical service providers. Examples include radiology, stroke assessment, mental health, and intensive care services.
- Monitoring center links used for cardiac, pulmonary or fetal monitoring, home care and related services that provide care to patients in the home. Landline or wireless connections are often used to communicate directly between the patient and the center while some systems use the Internet.
- Web-based e-health patient service sites that provide direct consumer outreach and services over the Internet.
The ATA estimates around 10 million Americans had a medical service provided remotely in 2013 although most were likely unaware of it. “It’s under the radar; you don’t even know it,” Linkous said. “It’s a seamless part of healthcare delivery.”
Telemedicine is most prevalent in the use of imaging. Often a radiologist reading an X-ray or MRI is located off site, even in another part of the world.
“Another example is neurophysiological monitoring for a patient undergoing back or brain surgery, people who look at brain waves,” Linkous said. “It’s not done in a hospital surgery room, it doesn’t need to be. It is done at a distance.”
About half of the physicians in the U.S. use a mobile app program that allows them to determine whether a medication they are considering prescribing interacts well with other drugs a patient is taking. That program, called Epocrates, is one of the more basic examples of telemedicine.
Some retail pharmacies that offer nurse-staffed mini clinics that provide checkups are beginning to offer them at a distance to avoid long waits. Someone with a rash, for example, can be seen remotely via technology by a physician who might be able to give a diagnosis.
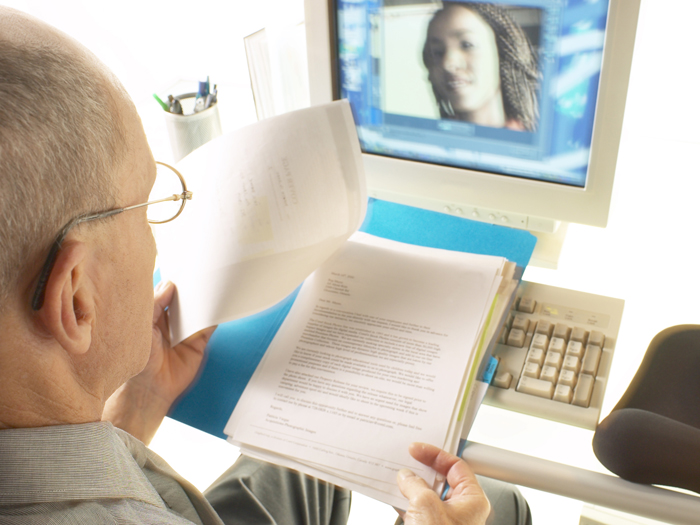
“It has advanced far beyond software, to provide the ability to see,” said Kimberly George, senior vice president, senior health care advisor, Sedgwick Claims Management Services Inc. “With Face Time and Skype, you can have a physical exam with the technology.”
Access to Care
The ability for health care to be provided without the requirement of a face-to-face meeting with a physician could potentially revolutionize health care delivery in the workers’ comp system. It provides several benefits.
“Top of the list is the Affordable Care Act and access to care,” George said. Telemedicine, she said, could be part of the answer to the potential shortage of physicians available to treat injured workers that could accompany implementation of the ACA — particularly in areas with few physicians.
“I’m from a rural town, and for years I’ve know how telemedicine is helpful for determining where the patient would be taken,” George said. “Rural is something that is definitely important in workers’ comp, and the timing of appointments, not just for seeing the occupational health [physician], but whether he should be seen by a specialist, and getting him there and [avoiding] the wait, and delayed return to work.”
Rather than having to wait to see various specialists such as physical therapists and orthopedic surgeons, telemedicine can expedite the process. Workers in the fast-food industry, for example, could be treated much more quickly via telemedicine.
“Burns are a potential need to be seen [by a specialist], but it may just need cream or ice while another may need to be seen,” George said. “With this technology, it’s a great way to say ‘does this patient need to be seen.'”
George also believes the ACA may create better educated health care consumers — yet another reason telemedicine could aid the workers’ comp system. “As we start to think about that whole level of efficiency and patients become more engaged as consumers, they become more demanding. So they aren’t necessarily going to sit back and wait for that visit.”
States that are more spread out geographically stand to gain the most from telemedicine at the moment. Nevada officials said with essentially only Las Vegas and Reno as areas with concentrated groups of physicians and specialists, telemedicine may provide health care delivery services more efficiently and cost effectively.
Team Advantage
Telemedicine offers even more than the ability to enable exams among providers and injured workers. It also provides an opportunity for multiple providers to confer about a claim.
“You could have the case manager, the physician, the physical therapist, and the patient — a live care plan conversation. … We are not too far away from being able to get there,” George said. “It’s really about access to care, but also that ability to have an efficient and timely visit by a specialist, and then the key stakeholders can really benefit from timely care and the patient feels ‘I’ve got the best providers and a system that is helping me get better,’ and avoiding delays.”
Technology offers workers’ comp the ability to move to the next level in the delivery of health care, especially for certain types of employers. The trucking industry is one example.
With 24/7 nurse triage, “what if that nurse has a physician that can do an evaluation within minutes to determine if the patient needs to be seen?” George said. “If you’ve got the right environment, where the truck driver is on the road and needs more than what the nurse can triage, could the equipment be in the truck or trailer and allow for medical review?”
Companies with on-site clinics could coordinate them with remote orthopedic or other occupational specialists. “A lot use nurse practitioners, but there are times you may want or need to have a physician. Could you block out time of telemedicine visits with occupational health specialists,” George said. “Those are opportunities.”
Chronic Health Conditions
The ability to monitor patients with conditions such as advanced diabetes, chronic obstructive pulmonary disease, or congestive heart failure can help prevent emergencies. That could potentially help injured workers with comorbidities.
“Often people with workers’ comp issues [and comorbidities] are in and out of emergency rooms once a week,” the ATA’s Linkous said. “There are many circumstances when people don’t go to a physician or at least get their vitals checked because they are in a far away location. This allows you to get that access.”
People with unchecked chronic diseases can wind up on disability or in rehabilitation facilities. “The potential cost savings through the use of telemedicine are huge for people who have chronic diseases,” Linkous said. “If you could monitor their condition on a regular basis, you could save lots of money.”
Sedgwick’s George takes it a step further and says telemedicine could help employers prevent the onset of chronic diseases among their employees. “Many people with chronic diseases or even pregnant women are using telemedicine and various mobile tools to focus on not just sick care but well care,” she said. “We’ve got to be thinking about that as employers.”
That goes to another potential benefit of telemedicine, the engagement of the employee, according to George. “Everybody wants an engaged employee — to show up, be well, participate in his recovery if injured,” she said. “The thought is that a telemedicine program could help improve engagement. It’s also believed it will reduce health care costs and needless disability tied to a decrease in costs in fewer ER visits.”
Ongoing Concerns
Despite the potential benefits, there is little discussion about telemedicine in the workers’ comp system. About 16 states have adopted mandates for the coverage of telemedicine with few considering it specifically for their workers’ comp systems.
“Health care compared to other industries is a late adopter of technology,” Linkous pointed out. “On the other hand, there is resistance to change. Physicians are paid quite well, and any type of change like this is perceived as a threat.”
There is also the issue of privacy. Face Time and Skype, for example, are not HIPAA compliant.
“It’s one thing to have a talk when a patient instigates that on their own,” George said. “But if a payer facilitates it, you have to make sure the equipment is secure and appropriate.”
There is also the issue of interoperability. “The equipment could be at the employer’s, and the physician doing the exam must have the [right] equipment,” George said. “With the provider and patient link, who pays and how do you get the patient and provider together?”
George said Sedgwick is addressing those issues and is nearly ready to roll out a pilot program. Despite the concerns, advocates believe it is incumbent on workers’ comp practitioners to embrace telemedicine.
“There are so many advancements in medical care. Telemedicine is a part of those advancements that, while unique to workers’ comp and evolving, is a major part of consumers today,” George said. “They may be going out to find information on the Web, they may be going to a health group website and getting medical information. So it’s an advancement in medical care that is not going to go away.”










