Sponsored Content by AmTrust Financial
This Clinically Focused Claims Program Is Taking Opioids Out of the Pain Management Equation

The opioid epidemic, though now well-recognized as a major public health crisis, continues to rage on as health care organizations, policymakers and local communities look for solutions.
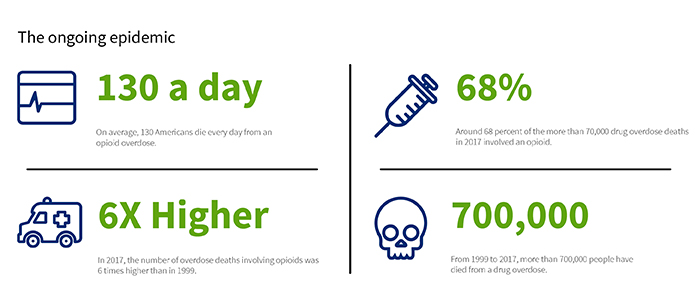
According to AmTrust Financial’s 2019 Opioid Prescription Risk Report, an average of 130 Americans die every day from an opioid overdose. The problem is particularly acute in workers’ compensation, where chronic pain is a common diagnosis among injured workers. National Council on Compensation Insurance (NCCI) data shows that in 2016, 44% of all workers’ comp claims with a prescription included at least one prescription for an opioid.
An overreliance on pharmaceutical interventions for pain has helped to fuel the epidemic, and a more proactive approach to identifying non-drug alternatives can help to end it. At least that is the theory driving a new utilization review program devised by workers’ comp carrier AmTrust Financial Services and its PBM partner Optum Workers’ Comp and Auto No-Fault.
Here’s how the clinically focused program is helping to get ahead of opioid addiction.
The Flaws of Pharma-Focused Pain Management
The opioid crisis can be traced to back to the early 1990s, when pain became the “fifth vital sign,” and pharmaceuticals became the primary treatment option.

Melissa Burke, Head of Managed Care and Clinical, AmTrust Financial
“Every day a nurse or doctor would go into a patient’s room and ask, ‘How’s your pain today?’ But the more you think about pain, the bigger it becomes,” said Melissa Burke, Head of Managed Care and Clinical, AmTrust Financial. “And just like you take a medication to fix high blood pressure or a high heart rate, we’ve conditioned ourselves to look for a similar cure for pain.”
This perspective on pain also feeds the fear that an injured worker experiences when entering the workers’ compensation system for the first time. For most, the process is unfamiliar. Claimants see doctors they don’t know and are unsure about, who is going to pay their bills, and who will take care of them and their families if they can’t return to work.
When health care providers prioritize pain, it becomes easier for patients to become fixated on their pain as well as an indicator of their long-term prognosis.
The drive to treat pain often leads to the early prescription of a high-strength painkiller. Oxycodone, fentanyl and morphine provide fast relief, assuaging injured workers’ fears and providing a false sense of recovery. Unfortunately, these drugs were never meant for long-term use.
“Relying on opioids means using an acute treatment to address a chronic problem,” Burke said. “Over time, this creates multiple additional problems for patients.”
Side effects from opioids include drowsiness, constipation, depression and anxiety, sexual dysfunction, and eventually, addiction. Patients often end up taking other medications to treat these effects.
“First they’re on something for bowel movement, then maybe they’re on something for nausea and vomiting, then they’re on a stimulant because they can’t stay awake during the day, then they’re on a sleeping pill at night because the stimulant won’t let them rest,” Burke said.
“Patients with a long-term opioid prescription could end up taking 10 additional drugs. It becomes a viscous cycle that ultimately results in poor outcomes.”
Applying Clinical Claims Expertise Early Makes a Difference
The key to prevent opioid use from spiraling out of control is to bring more scrutiny to the initial prescription, get injured workers on the most appropriate treatment path earlier, and hopefully keep them away from opioids altogether.
“Getting it right from the beginning is where it matters,” Burke said. “Ideally you want claim professionals who are very fluent in medication and pharmacy so they can better assess the medical need for an opioid prescription up front and suggest alternatives. But that’s much easier said than done.”
Other workers’ compensation carriers have in-house nurses to bring a clinical eye to claims, but don’t require a nurse to provide prior authorization on new opioid prescriptions. While adjusters do receive training in medical and pharmaceutical terminology and best practices, the learning curve is slow. To tackle the enormity of the epidemic, clinical decisions have to be made faster.
“We realized we had to bring medical expertise to the table earlier,” Burke said.
Through a partnership with pharmacy benefit manager Optum Workers’ Comp and Auto No-Fault, AmTrust was able to make that happen.

“Optum put together a unit of nurses who review any type of clinical edit on a claim. They are able to look at an initial prescription and the rest of the claim information to make an appropriate determination of medical necessity, proper dosage and prescription length,” Burke said.
“By routing those prescription authorizations directly to nurses, we can get ahead of the problem by spotting opportunities to use alternative pain management therapies. At the end of the day, we want to develop an individualized approach for each injured worker,” she said.
Simple sprains and strains, for example, can be treated with a nonsteroidal anti-inflammatory drug (NSAID), ibuprofen or acetaminophen. Non-pharmaceutical options like the RICE method (rest, ice, compression and elevation), massage therapy, yoga, physical therapy and exercise might also do the trick.
Increasingly, cognitive behavioral therapy has been shown to reduce pain by changing a negative mindset. For example, asking a patient, “What were you able to do today?” instead of “How is your pain?” takes the focus off a negative feeling and reroutes it to a focus on functional improvement.
“The nature of the injury, the way a person describes their pain, and other social and psychological factors would determine which type of treatment is most appropriate,” Burke said.
A Proactive Approach Shows Promising Results
This proactive and personalized approach to pain management has drastically reduced the prevalence of opioids among AmTrust’s workers’ compensation claims. In the fourth quarter of 2017, 60% of claims involved an opioid. In the fourth quarter of 2018, that figure fell to 25%.
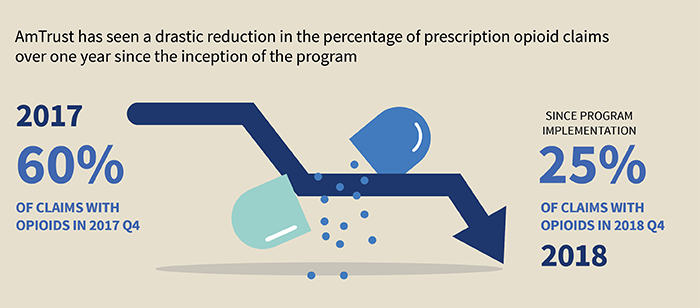
Prescription length has also dropped. Compared to a cohort of similar workers’ comp carriers, AmTrust’s average days’ supply of opioids per claim is nearly 38% shorter. The average MED per claim per day — which standardizes morphine dosage across various drug types including Oxycontin, Percocet and Tramadol — is also 63% lower compared to other insurers in the cohort.
“Overall, the program has prevented nearly 13,000 prescriptions that were either unnecessary or potentially unsafe,” Burke said.
Injured workers are not the only party that benefits from a proactive approach. Going to work under the influence of opioids presents a safety risk to a claimant’s co-workers as well.
“It’s not just the machine worker or truck driver — it’s everyone. Anyone on the job who’s on opioids is a risk to those around them. Our goal is to return injured employees back to work safely…not drowsy on a pain medication,” Burke said.
“Ultimately, avoiding opioid prescriptions in the first place produces a better outcome for injured employees, their colleagues and for society as a whole.”
To learn more, visit www.amtrustfinancial.com/opioids.
This article was produced by the R&I Brand Studio, a unit of the advertising department of Risk & Insurance, in collaboration with AmTrust Financial. The editorial staff of Risk & Insurance had no role in its preparation.










