Sponsored: Bardavon Health Innovations
How a Comprehensive Therapy Program Positively Impacts Injured Worker Recovery and Reduces Claim Costs

The workers’ compensation industry is facing several significant challenges today, including the rising costs of medical care and an increase in biopsychosocial issues that impact the workforce.
“This directly impacts claim costs,” said Jen Henry, director of clinical oversight, Bardavon.
As reported by the Bureau of Labor and Statistics, low back pain is the most common work-related musculoskeletal disorder across a variety of industries. Additionally, a recent WCRI study demonstrated that one-third of low back pain workers’ compensation claims had self-reported psychosocial issues, and half demonstrated fear-avoidance behaviors. This impacts such a large number of claims that it must be addressed.
The industry faces a pressing need for transparency and real-time data that can offer stakeholders actionable insights and information for better decision making regarding both physical and non-physical factors that impact a claim. And, of course, at the core of this is the injured worker, who is looking to recover and get back on the job.
One method that shows a net positive is physical therapy. PT plays a crucial role in treating workers’ compensation injuries and helps manage associated costs. Physical therapy, when prescribed early in the recovery process, can impact claims costs by 24 to 28%. Further, according to WCRI studies, early intervention in the form of physical therapy can avoid the need for surgical interventions, diagnostic procedures like MRIs, and stronger controlled substances.
However, there are several things to keep in mind when implementing a physical therapy plan: “Despite the use of PT positively impacting a claim, it still contributes to the overall cost, therefore it’s imperative organizations select the right therapy network partner to manage these claims effectively,” said Tiffany Gay, chief client officer, Bardavon.
“By taking a comprehensive approach that considers the injury, return-to-work goals, physical job demands and monitoring of the injured worker’s progress throughout care, we can intervene and provide insights to all stakeholders, ultimately saving claim costs” Gay said.
Understand the Worker’s Environment

Jen Henry, Director of Clinical Oversight, Bardavon
While physical therapy is a vital part of the workers’ compensation tool kit, a comprehensive therapy plan must consider the external factors that impact injured workers. Often, psychosocial factors will delay recovery if they’re not addressed.
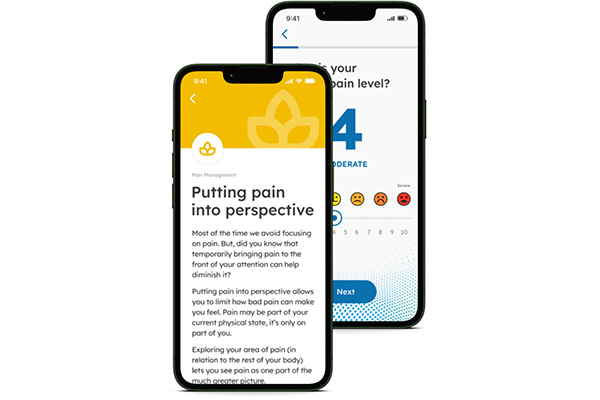
Enter Bardavon’s new Recovery+ program, a one-of-its-kind coaching platform that enhances our comprehensive in-person network therapy program and clinical oversight with routine check-ins via SMS with injured workers to support a fuller, faster recovery. Recovery+ engages injured workers to collect information on biological, psychological and social factors that may be impacting their recovery.
“Psychosocial issues play a significant role in recovery and return to work,” Henry said.
“Factors such as stress, anxiety, depression and lack of social support can all hinder the recovery process. These issues can lead to delayed healing, increased pain perception and a prolonged absence from work.”
Additionally, psychosocial factors influence an individual’s motivation and confidence in their ability to return to work. Kinesiophobia or the fear of reinjury, concerns about job security and perceived lack of support from employers or colleagues can all contribute to a reluctance to return to the workplace.
“By recognizing and addressing the role of psychosocial factors, we can create a more comprehensive and effective approach to injury recovery and return to work,” Gay said.
Bardavon is doing this already with its Recovery+ program, by assigning a clinical coach to every case. “On our side, this clinician reviews the information collected by the Recovery+ program, which includes patient-reported outcomes addressing biopsychosocial issues, functional deficits, pain and barriers to rehab,” Henry explained.
This psychosocial and self-perceived functional information is then passed along from coaches to stakeholders so the entire care team is aware of any issues that may impact recovery.
“Often, we have this information before the person even attends their initial therapy evaluation,” Henry said. “In some cases, we can contact the in-clinic therapist before the injured worker arrives for their appointment and provide them with relevant insights about the patient’s condition and potential challenges. This gets the care plan started on a successful path.”
Keep Top Clinicians Involved

Tiffany Gay, Chief Client Officer, Bardavon
Educating and arming the treating physician on what return to work looks like sets up both therapist and injured worker for success.
The Bardavon team understands that a comprehensive therapy plan requires provider education. If the treating clinicians are inexperienced in the workers’ compensation system, workers may face delayed recovery.
“We have always had a process for provider scoring that takes into account multiple factors. We assess how quickly an injured worker can start therapy, whether the therapist provides timely notes to all key stakeholders, and the quality of the physical therapist’s documentation,” Gay explained.
Clinicians who are educated in workers’ compensation needs can more effectively establish goals, help create a clear plan of care and a path toward return to work.
“With the introduction of Recovery+, our clinical coaches now interact with both the injured worker and the provider so that everyone is working toward a unified goal,” Henry said.
“The coaches review the charts from a workers’ comp-focused clinical perspective — assessing if the goals are return-to-work oriented, if the care plan involves job-specific simulations or work demand functional tasks, and whether it’s appropriate to recommend work conditioning, work hardening or a functional capacity evaluation,” she added.
The clinical coaches work with providers to enhance these skills – creating better outcomes, preventing delays in care, and prolonged claims cost.
The ultimate goal of the Recovery+ program is that, by deploying trained clinicians earlier into the PT scheduling process and equipping them with the language needed to navigate workers’ comp, there will be better management on the clinical, clerical and administrative complexities of the claim.
Meet Workers Where They Are
One final factor that any comprehensive therapy program should consider is integrating ways to better understand worker satisfaction throughout the process. That’s because understanding where the worker is, from both a recovery standpoint and how they are feeling, can contribute to better recovery results.
At its simplest, Recovery+ builds on the idea that increased injured worker engagement and communication creates the best possible return-to-work outcome.
“We know that the earlier someone gets into therapy, the better the chances are for a return to work and possibly a nonsurgical intervention,” said Gay. This early intervention is great news for payers because it can mean expedited referrals and lower costs.
It’s also a wonderful strategy to create injured worker satisfaction.
“Everyone wants to feel like their employer cares about their injury, recovery and personal wellbeing,” Henry said. “The sooner someone feels like they’re going to get help, the better.”
Another way Recovery+ places worker satisfaction at the fore is through customer satisfaction surveys from the injured workers. These surveys are distributed at the end of their first authorization period and again if treatment must extend beyond that.
“In these surveys, workers rate their care team members, including their physical therapist, nurse case manager and adjuster. We inquire whether the worker feels their employer cared about them, providing valuable feedback to our clients and payers about the level of support their employees perceive. It gives the injured worker a voice in their care,” Henry explained.
By sending and reviewing surveys throughout the process of care, Bardavon is constantly learning about its program and can make improvements as needed, further enhancing workers’ paths to recovery.
And the results are already speaking for themselves — 96% of injured workers surveyed to date are “satisfied” or “very satisfied” with the treating PT/OT from the Bardavon network, 81% said it was “easy” or “very easy” to schedule their appointments, and 71% were “satisfied” or “very satisfied” with their experience with the recovery program overall.
A Comprehensive Therapy Plan You Can Trust
The Bardavon network solution — which includes a national network of quality therapists, timely scheduling, clinical oversight and injured worker engagement via the Recovery+ program — keeps a pulse on each injured worker’s recovery plan, making sure that psychosocial factors are being addressed, that treating physical therapists are in tune with the worker’s individual needs and return-to-work plan, and that interventions are made when appropriate to keep claims on track.
“As part of our clinical oversight, we can identify appropriate discharge from care, getting them back to work better and faster, and increase the confidence level of both the payer and the injured worker that the risk of reinjury is low,” Henry added.
“At Bardavon, our mission statement is to impact the health and wellness of every worker, everywhere, and we strive to keep that person-centric focus at the forefront of our efforts,” Gay said.
To learn more, visit: https://www.bardavon.com/injury-recovery/.
This article was produced by the R&I Brand Studio, a unit of the advertising department of Risk & Insurance, in collaboration with Bardavon Health Innovations. The editorial staff of Risk & Insurance had no role in its preparation.










