Sponsored Content by CorVel
Ancillary Care Solutions: Uncovering the Key Factors of a Successful Program

The scheduling, coordination, and overall management of ancillary services make up a significant amount of medical spend in workers’ compensation. That is because an injured worker’s road to recovery is often complex, requiring clinical oversight and a high level of coordination for timely care delivery.
Ancillary services, which include physical therapy, diagnostic imaging, and durable medical equipment, are necessary in many cases to supplement primary care and can result in higher costs when treatment delays occur.
To gain insight into the current use of ancillary services and the most significant pain points risk managers face, CorVel sponsored a recent survey of industry professionals. The report identified key industry trends, analyzed areas of opportunity for improvement, and reported on the value of CorVel’s ancillary care solution, CareIQ.
How Ancillary Programs are Selected
The survey results showed that 60% of respondents do not currently use an ancillary network provider for their program. When asked what is a priority when selecting a partner, respondents ranked provider network savings, customer service, and the quality of treatment to employees as the top three factors. Additional considerations included provider network coverage, patient outcomes, ease of use, provider payment guarantees, and clinical oversight.
An effective program addresses all of these key factors, as the responsiveness of an ancillary services provider, network coverage, and the quality of care delivered to employees are crucial to achieving savings.
60% of respondents do not use an ancillary network provider.
Provider network savings is the most important consideration when choosing an ancillary services partner.
The Importance of Prompt Care
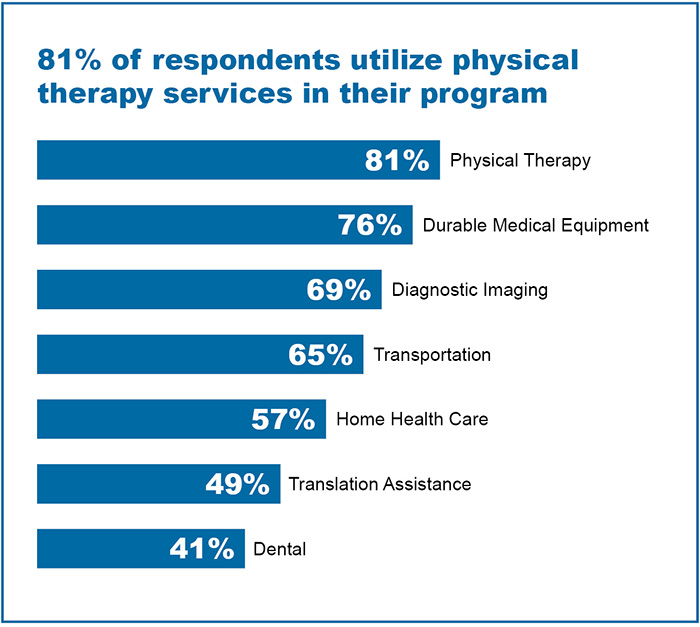
According to survey results, the most utilized ancillary services are physical therapy, durable medical equipment, and diagnostic imaging. Respondents provided insight into the challenges risk managers face today in utilizing these services in their workers’ compensation programs.
Delays in appointment scheduling and the overutilization of unnecessary treatment are top concerns. Multiple respondents noted the need for more streamlined communication between claims examiners, doctors, and employees as impacting timely scheduling, appropriate billing, and consistency of appropriate treatment.
Finding the right partner to streamline communication, provide network coverage, and provide timely care can address these pain points and improve program outcomes.

Evaluating Performance
In evaluating the performance of their current ancillary program, respondents ranked turnaround time, the average therapy visits per claim, and promptness of communication as the most important.

Top Tools and Trends
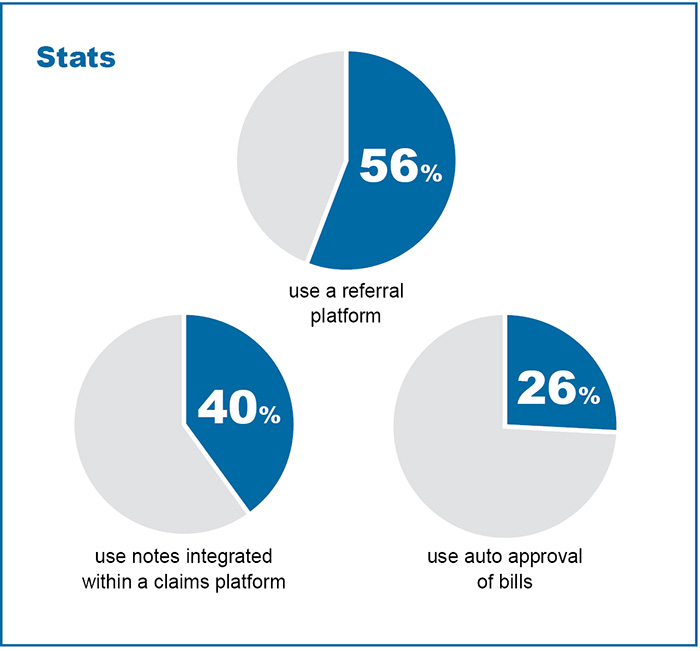
A referral platform is a tool most used by claims and case management staff to drive ancillary network utilization and referrals. Notes integrated within a claims platform and auto-approval of bills are also often used. This highlights the need for integrated, intuitive systems to increase utilization and referrals instead of relying on phone calls and email communications.
Survey results identified the trends the respondents observed in ancillary services that impact their business. One trend identified is the rising overall cost of services and costs per claim. Nearly half of all respondents estimated the percentage they spend on ancillary services is at least 20% of their program’s total medical costs. Respondents noted inflation, cost of increased utilization, and the quality of care management as key contributors to the rising costs their businesses experience.
Multiple respondents mentioned delays related to scheduling, immediate access to care, and claims processing. Other trends shared in the survey include inadequate network coverage and poor customer service.
Conclusion
The effective management of ancillary services is crucial to containing costs and achieving faster return to work. CorVel’s study found that diagnostic imaging, physical therapy, and other ancillary services can make up an average of 30% of a program’s medical spend. Having an experienced ancillary services provider, with the strategies in place to efficiently coordinate and deliver care, leads to better outcomes for both employers and their employees.
Key Findings Overview
- 60% of respondents do not use an ancillary network provider for their program.
- Appointment scheduling delays are the most significant pain point.
- 46% of respondents estimate that over 20% of their medical spend is related to ancillary services.
- Rising costs are the top trend observed by respondents that impact their business.
Please visit https://www.corvel.com/services/workers-compensation/ancillary-care-solutions/ to learn more about its ancillary care solutions.
This article was produced by the R&I Brand Studio, a unit of the advertising department of Risk & Insurance, in collaboration with CorVel. The editorial staff of Risk & Insurance had no role in its preparation.