Sponsored: Healthesystems
A New Paradigm for Pain Management: Thinking Beyond Opioids
It is time for workers’ compensation claims organizations to return to the fundamental principles of occupational medicine and shift the focus of care back to restoring function to injured workers. A new approach to pain management that goes beyond opioid therapy is needed, according to Robert Goldberg, MD, FACOEM, an occupational medicine specialist and chief medical officer at workers’ compensation PBM Healthesystems.
“Before opioid prescribing exploded in the workers’ compensation claim population, physicians focused on treating the injury and restoring as much function as possible so patients could return to work quickly. Today we see well-intentioned physicians prescribing opioids soon after an injury,” observed Dr. Goldberg. “That practice can actually impede recovery and return to work, and opens up patients, payers and employers to increased risks. The outcomes data show that this approach is not working. If payers make a fundamental shift back to a holistic treatment approach, the outcomes will improve for everyone.”
A catalyst for change
A new opioids treatment guideline developed by the American College of Occupational and Environmental Medicine (ACOEM) reflects new evidence and supports Dr. Goldberg’s assertion. It guides the use of medication for pain and discusses alternatives to the use of opioids. It also calls for a significant reduction in the recommended maximum morphine equivalent dosage (MED) from what was previously thought safe. Morphine is the standard against which the potency of other opioids is measured.
A past president of ACOEM, Dr. Goldberg expects the new guideline to serve as a springboard for payers to revisit and retool their pain management strategies, policies and procedures. “When physicians and payers recognize pain management as a tool that can enable patients to participate in treatment and recover, rather than thinking of it as the ultimate goal of treatment, they can begin to take a more comprehensive approach.”
The new evidence-based ACOEM opioids treatment guideline calls for prescribers to initially implement conservative pain management therapy by prescribing non-opioid drugs. Adjunctive therapies such as physical therapy, acupuncture, cognitive behavioral therapy, yoga and massage therapy can be considered if non-opioid therapies do not provide adequate relief. If pain persists, a short term of opioid therapy can be prescribed as long as appropriate screening and assessments have been conducted to guard against potential drug abuse, addiction or other factors that would contraindicate opioids.
“If payers make a fundamental shift back to a holistic treatment approach, the outcomes will improve for everyone.”
— Robert Goldberg, MD, FACOEM Chief Medical Officer, Healthesystems
Incorporate guidelines in policies and procedures
Payers need to develop new policies and procedures that incorporate the most current evidence-based guidelines, and work with their PBM to achieve a comprehensive, layered approach to patient care and pain management. Dr. Goldberg offers these considerations for retooling strategy:
- Engage in clinically supported discussions with prescribers. Providing educational information to physicians has proven to have a positive impact on prescribing patterns.
- Work with prescribers to set clear expectations with injured workers around pain relief, pain management and return to work. Patients will fare better if they are educated to expect that some pain may continue or even persist.
- Approve treatment with physical or occupational therapy to speed functional recovery.
- Approve alternative therapies to reduce reliance on pain medication. Cognitive behavior therapy, massage and yoga can help patients better cope with the presence of some pain. Adjunctive therapies can also include short courses of chiropractic and acupuncture.
- Approve a short course of opioid therapy only when appropriate, per evidence-based guidelines, such as when non-opioid and alternative therapies do not provide adequate relief.
Everyone benefits
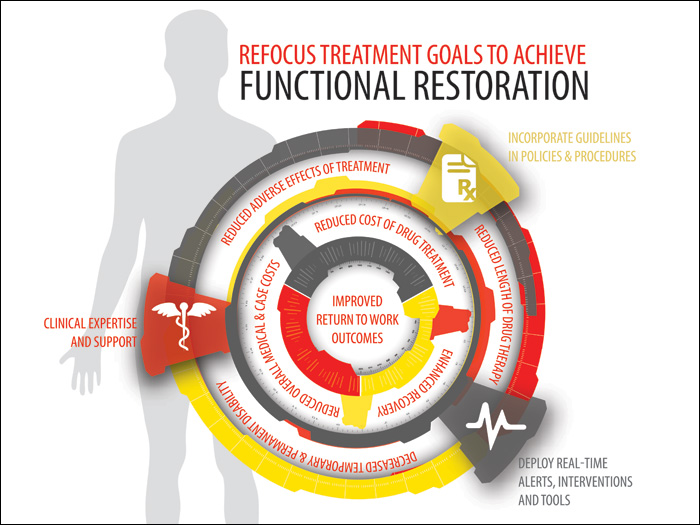
Such policies and procedures will help payers take a more holistic approach to patient care that goes beyond managing opioids. When the focus of care shifts to achieving functional improvement, the patient, payer and employer derive benefits that can include:
- reduced adverse effects of treatment
- reduced length and cost of opioid drug treatment
- decreased temporary and permanent disability
- enhanced recovery
- reduced overall medical and case costs
- increased likelihood that the injured worker will remain at work or return to work quickly
“Medical costs will inevitably come down with this approach because long-term opioid use will decrease and patients will be able to return to productive employment sooner,” commented Dr. Goldberg.
For more information on opioid strategies, read “Focus on the Patient, Not the Pain” and “Opioid Therapy: Effective Case Planning” in the Fall 2013 issue of Healthesystems’ RxInformer clinical journal. Request a subscription at www.healthesystems.com/rxinformer or access the latest issue on our iPad app in the App Store.
This article was produced by the R&I Brand Studio, a unit of the advertising department of Risk & Insurance, in collaboration with Healthesystems. The editorial staff of Risk & Insurance had no role in its preparation.










