Insurers: Are You Ignoring the Risk of Psychological Worker Injury at Your Own Peril?
The physical safety of employees is paramount to the operation of any workplace. Recently though, employers, claims handlers and employees themselves have increased their focus on psychological safety, what it means within the context of workplace wellbeing and managing risk.
Risk & Insurance® spoke with industry experts across the spectrum to discuss the types of psychological hazards that most often affect employees and what employers can do to mitigate these risks.
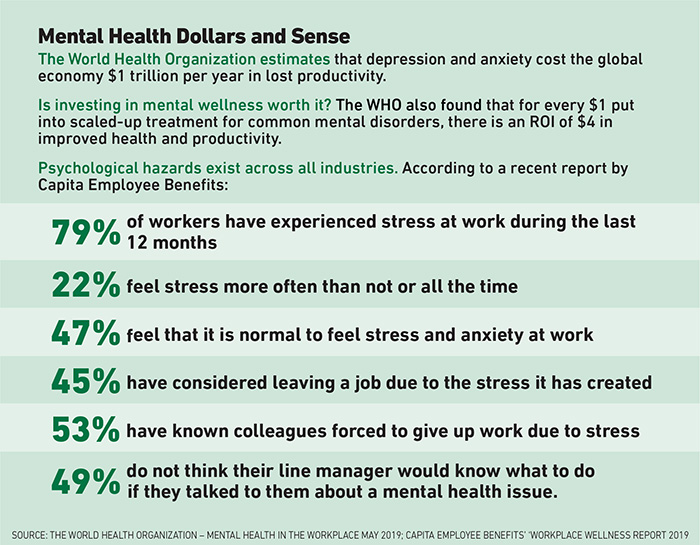
Psychological hazards take many forms, including serious chronic illnesses like post-traumatic stress disorder (PTSD). More commonly though, depression, burnout and anxiety due to workplace change and conflict are endemic.
According to the National Institute of Mental Health, nearly one in five Americans suffers from a mental illness, which was nearly 46.6 million people in 2017.
However, only about half of people with a mental illness of any kind receive treatment.

David Vittoria, senior vice president of clinical services, Carisk Partners
For David Vittoria, senior vice president of clinical services, Carisk Partners, this results in a variety of problems that carry over to the workplace. Vittoria is also a licensed clinical social worker and a trauma-trained and certified addictions, grief and recovery specialist.
“It’s important for us to keep in mind that the majority of these men and women suffering from depression, anxiety or substance use disorders, have jobs,” Vittoria explained.
“A lack of awareness about things like depression and anxiety is damaging to that injured worker first and foremost. It’s an adversarial and a confrontational position borne from ignorance that often leads to very costly consequences.
“I often hear that phrase: ‘We won’t buy the psych on this claim.’ My response is, ‘You already have.’ As states expand PTSD coverage for first responders, we’ll be forced to confront that.”
PTSD coverage for first responders hit mainstream news outlets after the 2016 Pulse nightclub mass shooting event in Orlando, in which police officers tasked with the initial search and recovery efforts were diagnosed with crippling PTSD symptoms that prevented them from returning to work.
As a result of this, Florida expanded coverage for so-called “mental-mental” claims for first responders. After a series of mass shootings in Texas, the state house made a similar move. Despite this expansion though, PTSD claims remain relatively rare.
Changing Times
Vittoria sees psychological hazards as stressors that tend to fall into three categories: organizational, environmental and personal. Some organizational hazards are issues like job security, workload, required pace and difficulty adapting to technological advancements.
Environmental factors might typically include things like indoor air quality, lighting or noise. But, he explained “it’s the personal factors that get overlooked and minimized. These are circumstances like change at work or at home, like a new boss or a child going away to college.”
Overall, industry leaders said that claims with a psychological component are on the rise, and this trend is expected to continue.
Christopher Shaeffer, CEO of Charles Taylor TPA, said PTSD claims are still usually associated with a major physical injury like an amputation, but that psychological components of a claim, like depression or anxiety, are an accelerating part of their claims handling.
“It’s a significantly increasing area that we’re seeing in our workers’ compensation claims,” Shaeffer said.
“We find it to be regional,” he continued. “We find it to be as little as 3% of claims in some places. In other regions, we see it as much as 15-20%. We have also increasingly accepted it as part of the injury process.”
“I often hear that phrase: ‘We won’t buy the psych on this claim.’ My response is, ‘You already have.’ ” — David Vittoria, senior vice president of clinical services, Carisk Partners
Shaeffer echoed Vittoria, confirming that the reticence to accept psychological components has changed dramatically in recent years.
“Generally, what needs to happen in the industry is that the adjusters and claims managers and the nurse case managers need to be more aware of this,” he said.
“Historically, workers’ compensation has shunned psychiatric aspects of claims. What we don’t know about or [can’t] get an X-ray to confirm, we are fearful of.”
That fear tends to extend to frontline managers in the workplace, who often lack the training, skills or awareness required to make employees feel safe. According to Dr. Maja Jurisic, medical director for Concentra, employers need to reframe how they think about the psychological elements of their workplaces.
“One of the big hazards is a lack of understanding among employers, and especially first-line supervisors, of how people are wired. The way we are wired is as emotional creatures who think, not thinking creatures who have emotions,” Jurisic said
Jurisic explained further that adverse interactions between supervisors and employees manifest as danger in the older part of our brain, triggering a flood of stress hormones, especially cortisol.
“Cortisol quite literally makes you stupid,” Jurisic said.
“It disables the executive function of your neo-cortex so you can’t think critically, you can’t learn new things, and you resort to what’s most comfortable and well-rehearsed.”
Monitoring Mental Health Is Possible
While some employers, especially those in heavy industry, are unable to control factors like the speed at which work is performed or mandatory overtime, there are some organizational changes that can be incorporated into the workplace.
Dr. Jake Lazarovic, chief medical officer of MyAbilities Technologies, along with Mike Sonne, VP of innovations and research at MyAbilities, developed a tool to assess the psychosocial factors of different occupations.

Dr. Maja Jurisic, medical director, Concentra
“What we have built into the MyAbilities platform is an automated psychosocial risk screening tool. It’s a validated tool with 13 questions,” Lazarovic explained.
“Based on the claimant’s responses to those questions, there’s an instant reading that indicates whether that individual is at high, medium or low risk for psychosocial barriers to recovery. And it furthermore indicates what interventions are recommended.”
Similarly, Paul Cassar, strategic director for mental health for Gallagher Bassett, recently launched a program called MyWellbeing, which clients can use to respond to an event that might result in mental injury claims.
Noting that where he is based in Australia mental injury claims are about 14% of their workers’ comp claims and expected to rise to up to 33%, Cassar explained this new program is meant to meet the challenge.
“The MyWellbeing plans are designed for that specific employee and their needs, to prevent them from experiencing a long-term illness or potentially being lost through staff turnover,” he said.
“Since we’ve launched that program in December, we’ve had 27 consults and 17 MyWellbeing plans drafted, and we haven’t had one mental injury claim result out of those interventions.”
The plans seek to address factors like work design, job control, role clarity and communication around the way employees go back to work.
How Effective Are Wellness Programs?
Overall, experts say that while wellness or employee assistance programs can help, they are often too general or underfunded to help most people struggling under the weight of psychological hazards at work.
As Sonne explained, “If you implement a psychological wellness program in a workplace, yet you still constantly expose that person to psychosocial stressors, I doubt that the wellness programs will be effective.”
Terri Rhodes, CEO of Disability Management Employer Coalition (DMEC), agreed.
“There’s been a lot of talk about EAP programs. And while their intent is good and they may help employees get easier access, I think we need to make sure that we have adequate benefits in our health plans. Access to care is a national crisis,” she said.
As claims managers, employers and employees continue to develop an awareness of the range of psychological hazards in the workplace, whether organizational, environmental or personal, the onus will be on everyone to reduce the likelihood that workers are lost in the shuffle.
As Vittoria emphasized, “If you couple the symptoms of psychological disorders with stigma, it can seem like there’s no way out.” &