Pharmacy Trends
Ecstasy as PTSD Treatment: Will You Be Footing the Bill?
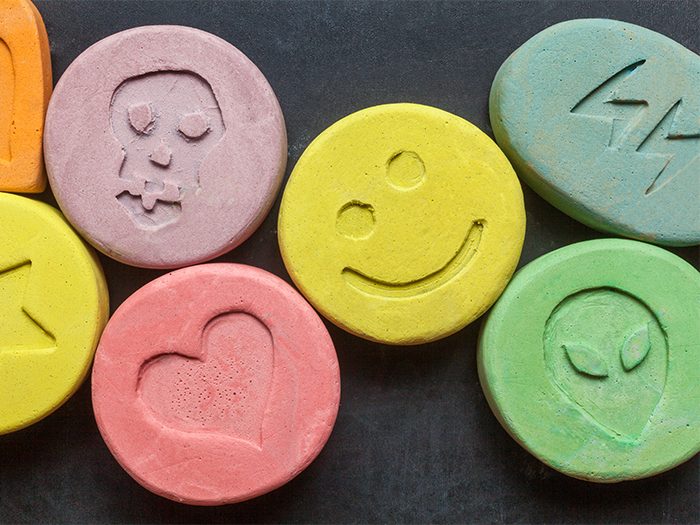
With medical marijuana being used more frequently in the treatment of workers’ comp patients, ecstasy — widely known as a rave-culture party drug — may be next.
Researchers found that two doses of ecstasy, termed 3,4-methylenedioxymethamphetamine, or MDMA — in conjunction with psychotherapy — reduced the post-traumatic stress disorder (PTSD) symptoms of 26 veterans and first responders in a “Phase 2” trial, according to a study published in the British journal The Lancet Psychiatry.
The Food and Drug Administration has already given MDMA “breakthrough therapy status” based on earlier results, which could expedite approval, The New York Times writes. Larger, “Phase 3” trials are set to start this summer, and if all goes well, the drug could be approved for legal use by 2021.
A small number of states, including Colorado, Vermont and Texas, cover PTSD under their workers’ compensation statutes. But recent mass tragedies such as the Santa Fe High School shooting have brought renewed focus to the impact of such events on emergency personnel.
Florida and Minnesota both passed bills this year that will allow workers’ comp benefits for first responders with PTSD injuries. A measure in New Hampshire is under consideration.
As more states follow suit and PTSD claims rise, does the potential acceptance of MDMA worry workers’ comp professionals at all? It’s complicated, experts say.
“The first concern I had upon reading about the potential use of ecstasy for treatment of PTSD is whether this could further open up Pandora’s box, especially at a time when drug abuse is on the rise,” said Lisa M. Haug, director of medical management, Safety National, in St. Louis.
Haug is also concerned about the long-term effects of such treatment, the potential side effects and the costs. However, on the flip side, the limited study showed some potential when the drug was being used under a very controlled environment in conjunction with psychotherapy.
“While it is too early to consider ecstasy as a treatment option in workers’ compensation, we cannot say it would never be deemed appropriate,” she said. “It was not that long ago that people felt medical cannabis had no role in workers’ compensation, and now we have seen several states order this treatment and some patients have positive results with it.”
Dr. Robert L. Goldberg, chief medical officer, PBM Healthesystems, in Tampa, Fla., said the research shows a high degree of efficacy with the treatment level dosing, as compared to the control low dose of MDMA that was provided.
“Shown in a small group, this can be very effective — when paired with psychotherapy, which is the really important distinction here,” Dr. Goldberg said.
Secondly, the research study was small — a Phase 2 trial with only 26 patients, he said. As such, both the medical community and the workers’ comp community should not get “too excited” either positively or negatively about MDMA being adopted as a treatment until larger Phase 3 trials are undertaken.
“Many times in smaller trials, you do get good results and lower incidence of side effects, but the results of the complete trial might not be quite as good, or the side effects profile might become more apparent,” Dr. Goldberg said.
Standardization Will Speed Acceptance
Some of the concerns about how medical marijuana is currently “administered” — in the loosest sense of that word, could spill over to the use of ecstasy in workers’ comp claims — that is, unless the drugs can be standardized, he said.
“With medical marijuana, it’s all self-dosing, even within a workers’ comp claim,” he said. “In a handful of states, the courts have decided that payers have to be reimbursed for medical marijuana if it was based on a recommendation by a physician, though in some states it’s by a designated expert, not just the treating physician. Yet the amount of marijuana is variable, so payers are still obligated while there’s no standardization for dosage or cost.”
“The first concern I had upon reading about the potential use of ecstasy for treatment of PTSD is whether this could further open up Pandora’s box, especially at a time when drug abuse is on the rise.” — Lisa M. Haug, director of medical management, Safety National
New Mexico set a maximum reimbursement level, but not for dosage. The good news, Dr. Goldberg said, is that once a dosage standard is established, medical marijuana will be manufactured just like any other medication in the U.S., enabling doctors to more easily prescribe and dispense the drug.
The same could be true for MDMA, though the route could be quicker, he said. Once it becomes scheduled, it will likely be a Schedule 2 or 3 drug. However, people who are self-dosing outside of clinical trials “really won’t know what they are getting on the street” — the drug may have other hallucinogens, contaminants or adulterants in it.
“But there’s a clearer path with MDMA and these trials, which could result in it being manufactured much more quickly with the proper processes, just like any standard medications such as ibuprofen,” Dr. Goldberg said.
“However, you’ll still have the same issues as with medical marijuana about how long the effects are going to last and if you can function at work after taking the medication,” he added. &











