Sponsored Content by Helios
Medication Monitoring Achieves Better Outcomes
There are approximately three million workplace injuries in any given year. Many, if not the majority, involve the use of prescription medications and a significant portion of these medications is for pain. In fact, prescription medications are so prevalent in workers’ compensation that they account for 70% of total medical spend, with roughly one third being Schedule II opioids (Helios; NCCI; WCRI; et al.). According to the U.S. Drug Enforcement Administration (DEA), between the years of 1997 and 2007, the daily milligram per person use of prescription opioids in the United States rose 402%, increasing from an average of 74 mg to 369 mg. The Centers for Disease Control and Prevention (CDC) reports that, in 2012, health care providers wrote 259 million prescriptions—enough for every American adult to have a bottle of pills—and 46 people die every day from an overdose of prescription painkillers in the US. Suffice to say, the appropriate use of opioid analgesics continues to be a serious issue in the United States.
Stakeholders throughout the workers’ compensation industry are seeking solutions to bend the curve away from misuse and abuse and these concerning statistics. Change is happening: The American College of Occupational and Environmental Medicine (ACOEM) and the Work Loss Data Institute have published updated guidelines to promote more clinically appropriate use of opioids in the treatment of occupational injuries. State legislatures are implementing and enhancing prescription drug monitoring programs (PDMPs). The Food and Drug Association (FDA) is rescheduling medications. Pharmaceutical manufacturers are creating abuse-deterrent formulations. Meanwhile payers, generally in concert with their pharmacy benefit manager (PBM), are expending considerable effort to build global medication management programs that emphasize proactive utilization management to ensure injured workers are receiving the right medication at the right time.

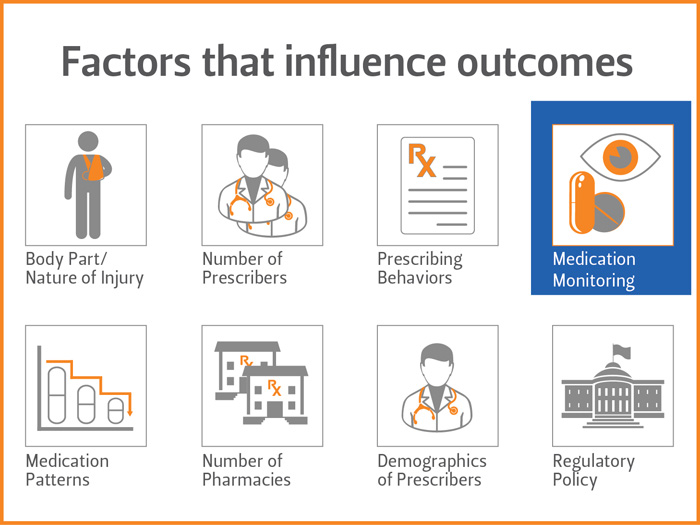
A variety of factors can still influence the outcome of a workers’ compensation claim. Some are long-recognized for their affect on a claim; for example, body part, nature of injury, state of jurisdiction, and regulatory policy. In contrast, prescribing practices and physician demographics are perhaps a bit unexpected given the more contemporary data analysis showing their influence on outcomes. Such is the case for medication monitoring. Medication monitoring tools promote patient safety, confirm adherence, and identify potential high-risk, high-cost claims. Three of the more common medication monitoring tools include:
- Urine Drug Testing (UDT) is an analysis of the injured worker’s urine that detects the presence or absence of a specified drug. Although it is not a diagnosis, UDT results are generally a reliable indicator of what is present (and what is not) in the injured body worker’s system. The knowledge gained through the testing helps to minimize risks for undesired consequences including misuse, abuse, and diversion of opioids. With this information in hand, adjustments to the medication therapy regimen or other intervention activities can occur. UDT can also be an agent of positive change, as monitoring often leads to behavior modification, whether in direct response to an unexpected testing result or from the sentinel effect of knowing that medication use is being monitored.
- Medication Agreements or “Pain Contracts” signed by the injured worker and their prescribing doctor serve as a detailed and well-documented informed consent describing the risks and benefits associated with the use of prescription pain medications. Medication agreements help the prescribing doctor set expectations regarding the patient’s adherence to the prescribed medication therapy regimen. They serve as a means to facilitate care and provide for a way to document mutual understanding by clearly delineating the roles, responsibilities, and expectations of each party. Research also suggests that medication agreements promote safety and education as injured workers learn more about their therapy regimen, its risks, and benefits.
- Pill Counts quantify adherence by comparing the number of doses remaining in a pill bottle with the number of doses that should remain based on prescription instructions. Most often, physicians request pill counts at random intervals or the physician may ask the injured worker to bring their medication to all appointments. As a monitoring tool, pill counts can be useful in confirming proper use, or conversely, diversion activities.
On a stand-alone basis, these tools rank high on individual merit. When used together as part of a consolidated medication management approach, their impact escalates quite favorably. The collective use of UDT, Medication Agreements, and pill counts enhance decision-making, eliminating gaps in understanding. Their use raises awareness of potential high-risk, high-cost situations. Moreover, when used in concert with a collaborative effort on the part of the payer, PBM, physician, and injured worker, they can improve communication and align objectives to mitigate misuse or abuse situations throughout the life of a claim.
Medication monitoring can achieve better outcomes
The vast majority of injured workers use medications as directed. Unfortunately, situations of misuse and abuse are far too common. Studies show a growing trend of discrepancies between the medication prescription and actual medication-regimen adherence when it comes to claimants on opioid therapy (Health Trends: Prescription Drug Monitoring Report, 2012). In response, payers, working alongside with their PBM and other stakeholders, are deploying medication monitoring tools with greater frequency to verify the injured worker is appropriately using their medications, particularly opioid analgesics. The good news is these efforts are working. Forty-five percent of patients with previously demonstrated aberrant drug-related behaviors were able to adhere to their medication regimens after management with drug testing or in combination with signed treatment agreements and multispecialty care (Laffer Associates and Millennium Research Institute, October 2011).
In our own studies, we have similarly found that clinical interventions performed in conjunction with medication monitoring tools such as UDT reduces utilization of high-risk medications in injured workers on chronic opioid therapy. Results showed there was a decrease in all measures of utilization, driven primarily by opioids (32% decrease) and benzodiazepines (51% decrease), as well as a 26% reduction in total utilization of all medications, regardless of drug class. This is proof positive that medication monitoring can be useful in achieving better outcomes.










