Sponsored: myMatrixx
9 Critical Capabilities for a Modern PBM Claims Management System
Managing workers’ compensation claims can often be overwhelming. Claims representatives already have notoriously heavy workloads, and the lack of sophistication and reliability of many tools available to them certainly doesn’t help.
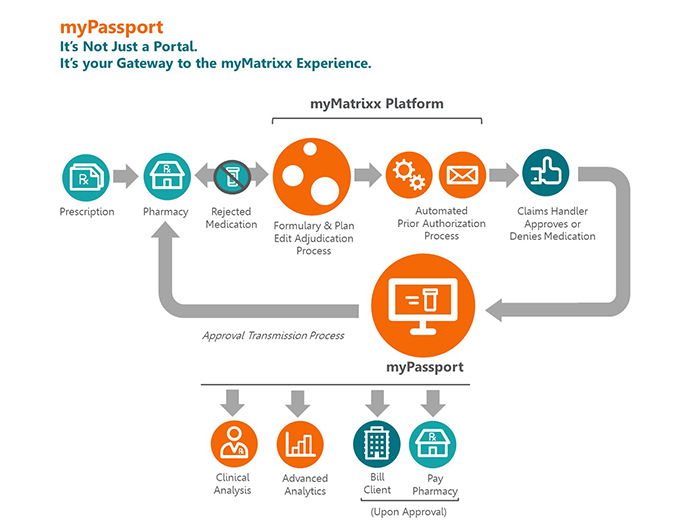
One of the many complex aspects of managing a claim is the pharmacy component. Determining the appropriateness of a claimant’s prescription and monitoring its ongoing usage, as the injured worker rehabilitates, is key to both controlling costs and ensuring optimal clinical outcomes. Pharmacy benefit managers, therefore, are crucial partners in the claim management process.
Most PBMs offer an online portal where their clients can access prescription information and centrally manage their claims. However, those portals largely haven’t kept up with advances in technology. More often than not, they are difficult to navigate, require many unnecessary steps, don’t contain comprehensive clinical information, and in general are not very helpful beyond basic authorization capabilities.
“We know that the front-line claims examiner has a mountain of responsibilities and pharmacy is just one piece of it,” said Hollie Lamboy, Vice President of Product Development for pharmacy benefit manager myMatrixx. “We saw an opportunity to make the lives of front-line claims examiners easier by providing efficiency and overall a more positive experience. Our goal is to lift the workload and simplify their job while providing easier access to data analytics and comprehensive information.”
myMatrixx began work on a new and improved PBM tool that embeds these nine best-in-class characteristics:
1. Ease of Use

Hollie Lamboy, Vice President of Product Development, myMatrixx
All the advanced capabilities in the world don’t matter if they are too inconvenient and cumbersome to bother with. An effective portal should be intuitive and easy to use. A simple and streamlined design makes it easy for new users to navigate.
“The end user should be able to do what they need in just a few steps. It should not be overwhelming or time-consuming. Simple and easy functionality is important,” Lamboy said.
2. Configurable and Scalable to Your Workflow
Pharmacy management tools should help claims representatives do their job, not force them to fit their processes into a rigid, predefined workflow. Likewise, a PBM portal should be configurable and adaptable to accommodate any user’s needs and the sophistication of their organization.
“A good tool isn’t one-size-fits-all. It should grow as the client grows and be able to configure to client operations, not vice-versa,” Lamboy said. “To that end, it needs a degree of customization.”
3. Provides Comprehensive Information
The ongoing opioid epidemic shines a light on the critical nature of pharmacy decisions. If a doctor wants to prescribe a high-strength painkiller, it’s incumbent upon the claims representative to fully understand whether or why that drug is really necessary, what dosage is appropriate, how long the patient should be on it and what steps should be taken if anything if the prescription plan goes awry.
Decisions based on incomplete or inaccurate information can have harmful and long-term effects on claimants’ lives and cause a claim to snowball out of control.
“Claims examiners can better monitor patient safety by knowing all the drugs that the patient is taking and understanding their purpose and contraindications. A tool should provide access to comprehensive prescription information so the examiner doesn’t have to look elsewhere or engage in conversations to obtain the needed information,” Lamboy said.
4. Helps Deliver Clinical Messaging
Seasoned adjusters and claims managers may be quite familiar with injury etiology and medical terminology, but those that don’t come from a clinical background may need additional clarification or help deciphering clinical communications.
“If you’re not a clinically-inclined person, myPassport should help by providing clinical messaging so that the claims examiners can break down and understand what a drug is used for, what type it is and if there are any red flags you need to be concerned about,” Lamboy said.
5. Keeps Patient Data Private and Secure
Protecting patient information is paramount. Unauthorized access violates patient privacy and can have significant liability implications for the claim management organization and the PBM.
“You want to make sure that all the necessary protocols are in place to ensure the information you’re viewing is secure and that access to the tool is secure,” Lamboy said. “At myMatrixx, we’ve taken rigorous steps to ensure the data is protected. It has to be bulletproof.”
6. Stores Relevant Documents
PBMs take on an important role of physician and patient outreach, ensuring that doctors prescribe responsibly and that patients understand and adhere to the mediation protocol. Claims representatives need to keep track of the communications and actions happening throughout the life of a claim.
A tool that centrally houses relevant documents and communications in one place allows claims personnel quick and easy access to all claim activity, which helps them stay updated on the claimant’s progress and enables them to intervene at the right time if necessary.
7. Let’s You Chat with Experts Instantly
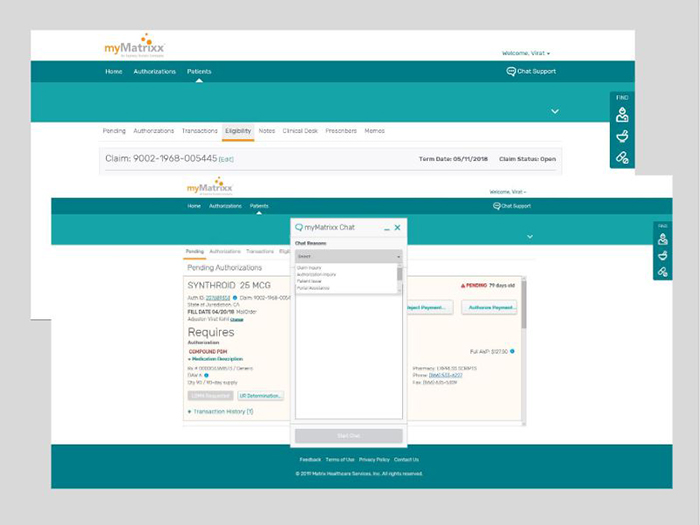 We all know the annoyance of hunting down a phone number or email address and having to open up a new conversation to ask a simple and straightforward question. The time spent finding a contact and waiting for a response is time wasted. Online chat functions allow for an immediate answer from a qualified expert.
We all know the annoyance of hunting down a phone number or email address and having to open up a new conversation to ask a simple and straightforward question. The time spent finding a contact and waiting for a response is time wasted. Online chat functions allow for an immediate answer from a qualified expert.
“It goes back to ease of use. Chat tools embedded in myPassport offer prompt and direct communication, and claims representatives don’t have to leave what they’re doing while getting an answer to a question,” Lamboy said.
8. Personalizes Access Control
Self-administrated password management at the individual level matters when it comes to ease of use. The ability to manage an account without administrator involvement means work gets done faster and with less frustration. Likewise, single sign-on capability means less time spent recovering or resetting a password every time it’s forgotten.
9. Works on any Device
Portals should be accessible and functional from whatever device or platform a claims representative is using — a 22-inch desktop computer, tablet, iPhone or Android phone.
“You won’t need to download an app. The idea is that claims representatives open a browser and log in and no matter what device or operating system you’re using, myPassport will adapt and work in the same manner without compromising ease-of-use,” Lamboy said.
A New and Improved Solution Takes Shape
When myMatrixx and Express Scripts merged, we took the best of both client portals and made additional improvements to fix the common challenges that adjusters run up against each day. Now we have a solution that is better than anything else out there,” Lamboy said. “We knew we could not develop a cookie-cutter solution. So we didn’t.”
Lamboy and her team assembled client focus groups to learn exactly what is needed in a PBM tool. “It’s a collaborative process that engages our clients. Their feedback is an integral part of the process,” she said. Continual feedback is also collected and used to improve myPassport. Though so far, comments have only been positive. “Claims examiners have begun using myPassport with no interruption to their workflow, and that’s been our goal from day one: to make it seamless and easier,” Lamboy said.
Implementation is seamless. After an initial registration and training process, every authorized user can access to their designated claim data.
To learn more, visit www.mymatrixx.com.
This article was produced by the R&I Brand Studio, a unit of the advertising department of Risk & Insurance, in collaboration with myMatrixx. The editorial staff of Risk & Insurance had no role in its preparation.










