On-Demand Webinar
Insurtech & Talent Crisis Crossroads: How successful claims operations maximize next generation technology & talent
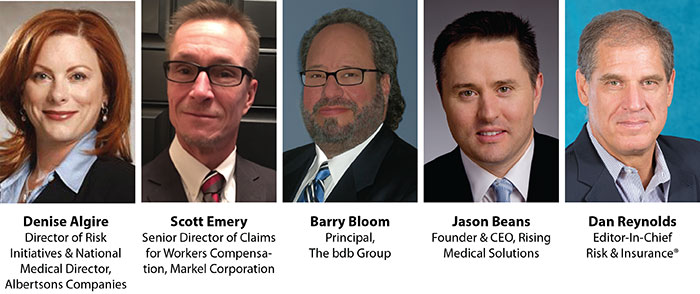
Presenters
Overview

Webinar Sponsor
Industry narratives about Insurtech’s disruption as well as the claims talent crisis are so constant that they might numb any sense of urgency via alarm fatigue. But these game changers are real and organizations that ignore them risk performance failure.
Herein lies the opportunity: Younger workers are attracted to jobs that fulfill their need for social justice and compassion. They also arrive tech ready, which dovetails neatly with the workers’ compensation sector’s need for claims adjusters who are primarily advocates for injured workers and who are equipped to marshal artificial intelligence and predictive analytics — dubbed Insurtech — to produce better claims outcomes.
Thus, how to recruit and train tech-ready talent and refit claims organizations to satisfy the younger workers’ need to make a positive impact on their society is a challenge facing every payer’s claims leadership.
In this one-hour webinar, experts from the fifth annual Workers’ Compensation Benchmarking Study will discuss how high-performance claims organizations are deftly navigating, and even maximizing, the intersecting crossroads of Insurtech and the talent recruitment/retention shortage. That conversation will focus on…
- Challenges and opportunities Insurtech presents for claims adjusters and how high-performance organizations are using best practices to ensure and propel results.
- How claims talent recruitment and desirable skills are changing right in front of our eyes.
- Using scenario-based learning and other tools to advance advocacy-based claims management techniques.
- How to sell organizational leadership on the vital importance of devoting more resources, not less, to claims management training and competency monitoring.
Webinar attendees will receive complimentary copies of the 2017 Benchmarking Study Report and the study group white paper “Do 10,000 Hours Make a Great Claims Professional?”.
Who should attend this webinar?
- Adjusters
- Risk Managers
- Case Managers
- Claims executives
- Medical directors
- Workers’ compensation underwriters
- Workers’ compensation legal experts
Recording
Download a PDF slide deck of the presentation.










